Explaining Charcot Foot

Charcot foot is a serious condition that affects the bones, joints, and soft tissues of the foot and ankle. It is most common in people with diabetes who have peripheral neuropathy. Charcot foot leads to inflammation that weakens the bones, making them more prone to fractures and dislocations. Because neuropathy reduces sensation, people may continue walking on an injured foot without realizing the extent of the damage. Over time, this can cause severe deformities, such as a collapsed arch, known as a rocker-bottom foot. Symptoms often include swelling, warmth, redness, and changes in foot shape. Without proper treatment, Charcot foot can increase the risk of wounds and infection, which may lead to limb loss. A podiatrist can assess the condition using imaging studies and clinical evaluations. Treatment typically involves immobilization with a cast or brace to prevent further damage. In more severe cases, surgery may be needed to restore foot stability and function. If you believe you have symptoms of Charcot foot, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Some foot conditions may require additional professional care. If you have any concerns, contact Dr. Ronald K. Olm of Grand Traverse Foot & Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact one of our offices located in Traverse City and Kalkaska, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Rare Foot Conditions
A podiatrist will be able to address a variety of rare foot conditions, particularly the ones that affect children. The most common are Kohler’s disease, Maffucci syndrome, and Freiberg’s disease. They can be properly diagnosed by having an X-ray taken, but in more serious cases an MRI may be needed. Kohler’s disease generally affects younger boys and bone deterioration may result from an interruption of blood supply. Children who have Kohler’s disease may find relief when the affected foot is rested, and a special boot is worn. Benign growths in the long bones of a child’s foot may lead to the development of bone lesions, and this is known as Maffucci syndrome. People who have this condition find mild relief when custom-made orthotics are worn. Freiberg’s disease targets the ball of the foot and can typically affect pre-teen and teenage girls. The metatarsal bone becomes deteriorated and flattened, and common symptoms include swelling and stiffness. A cast is often necessary to wear with this disease as it can help to reduce existing pain. Erythromelalgia is a rare foot condition, and its cause is unknown. Symptoms of this disease can include intense burning pain and the feet may appear red or feel warm. Relief may be found when the affected foot is immersed in ice water. It can also be beneficial to elevate the foot frequently. If your child complains of foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rare foot conditions.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
Arthritis Can Cause Pain in the Feet and Ankles
Achilles Tendon Injuries in Cyclists

Achilles tendon injuries are a frequent concern for cyclists due to the repetitive motion and sustained force placed on the lower leg. The Achilles tendon connects the calf muscles to the heel bone, and excessive strain can lead to inflammation or degeneration. Poor bike fit, improper cleat placement, and muscle imbalances may increase the likelihood of an Achilles tendon injury, particularly when the heel or toes are forced into an unnatural position while pedaling. Symptoms include stiffness, swelling, and pain near the heel or along the tendon, which may worsen in the morning or after cycling. People with tight calf muscles or restricted ankle mobility may also be at higher risk, as limited flexibility can cause additional strain on the tendon. A podiatrist can evaluate your foot and ankle mechanics, recommend custom orthotics to improve alignment, and provide treatment to reduce pain and promote healing. Severe cases may require surgery to repair tendon damage. If you are experiencing Achilles tendon pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment options.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Ronald K. Olm of Grand Traverse Foot & Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Traverse City and Kalkaska, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
A Simple Guide for Foot Wound Care

Foot wounds can lead to serious complications if not cared for properly. A podiatrist is a trained specialist who takes specific steps to clean and treat a foot wound to ensure it heals effectively and reduces the risk of infection. After the hands are washed, the wound is assessed for any foreign debris, such as dirt or stones. Using sterile gauze or a clean cloth, the wound is cleaned with mild soap and water, and caution is taken to not scrub the affected area. This is followed by applying a suitable antiseptic solution to disinfect the wound. Once the area is properly cleaned and disinfected, the wound is covered with a sterile bandage to create a protective barrier, promoting faster healing. If you have sustained a foot wound, it is suggested to seek professional care from a podiatrist to ensure the wound is treated appropriately and to receive guidance on the best care practices for your specific injury.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Ronald K. Olm from Grand Traverse Foot & Ankle Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Traverse City and Kalkaska, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Symptoms and Risk Factors of Heel Spurs
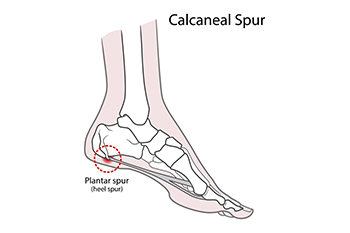
A heel spur is a bony growth that forms on the underside of the heel bone, often caused by long-term strain on the foot’s ligaments and muscles. This condition usually develops as a result of repetitive stress, such as excessive walking or running, which can lead to inflammation and the formation of calcium deposits. The primary symptom of a heel spur is sharp pain, especially when standing or walking after long periods of rest. The pain may decrease as the foot warms up, but it can return with prolonged activity. Risk factors for developing a heel spur include having flat feet, being overweight, wearing poorly fitting shoes, or engaging in activities that put excessive pressure on the feet, like running on hard surfaces. Additionally, people with conditions like arthritis or diabetes may also be at a higher risk. If you have heel pain, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and appropriate treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. Ronald K. Olm from Grand Traverse Foot & Ankle Center. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Traverse City and Kalkaska, MI . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.